You may have heard of IVF, but have you heard of PGT? Trying to conceive (TTC) can be challenging but learning about the common methods and technologies used in the world of fertility shouldn’t be. Let’s take a step back and go over common fertility terms and acronyms.
IVF, IUI, and Infertility
In vitro fertilization (IVF) is when an egg is fertilized by sperm outside of the body. Infertility (IF) is a common reason for IVF use. Infertility is defined as when a couple cannot conceive after one year of regular, unprotected sex. When this occurs, they might turn to ART or assisted reproductive technology. ART is any procedure where both the eggs and sperm are handled. Since IVF involves fertilizing eggs with sperm outside of the body, it is one form of ART. Two other forms include Intrauterine insemination (IUI) and Intracytoplasmic sperm injection (ICSI). IUI is when sperm is introduced into the uterus, using a medical device to increase the chances of fertilization. ICSI is when an embryologist selects one sperm to inject into one egg. This is helpful when sperm quality is low and cannot penetrate the egg on its own.
Oocytes and Ovarian Reserve
IVF involves retrieving the eggs (also called oocytes) from a woman’s ovaries through oocyte retrieval (OR) where a needle will retrieve the eggs from ovarian follicles. The needle is guided by an ultrasound probe as it is inserted through the vaginal wall to reach the ovarian follicle.
You will probably hear a lot about “ovarian reserve” when discussing egg/oocyte retrieval with your provider. This term is used to refer to the number and quality of eggs a woman has left in her ovaries, an indication of reproductive potential. When someone has diminished ovarian reserve (DOR), it means their reproductive potential is reduced due to a lower amount and/or quality of eggs remaining.
Preimplantation Genetic Testing
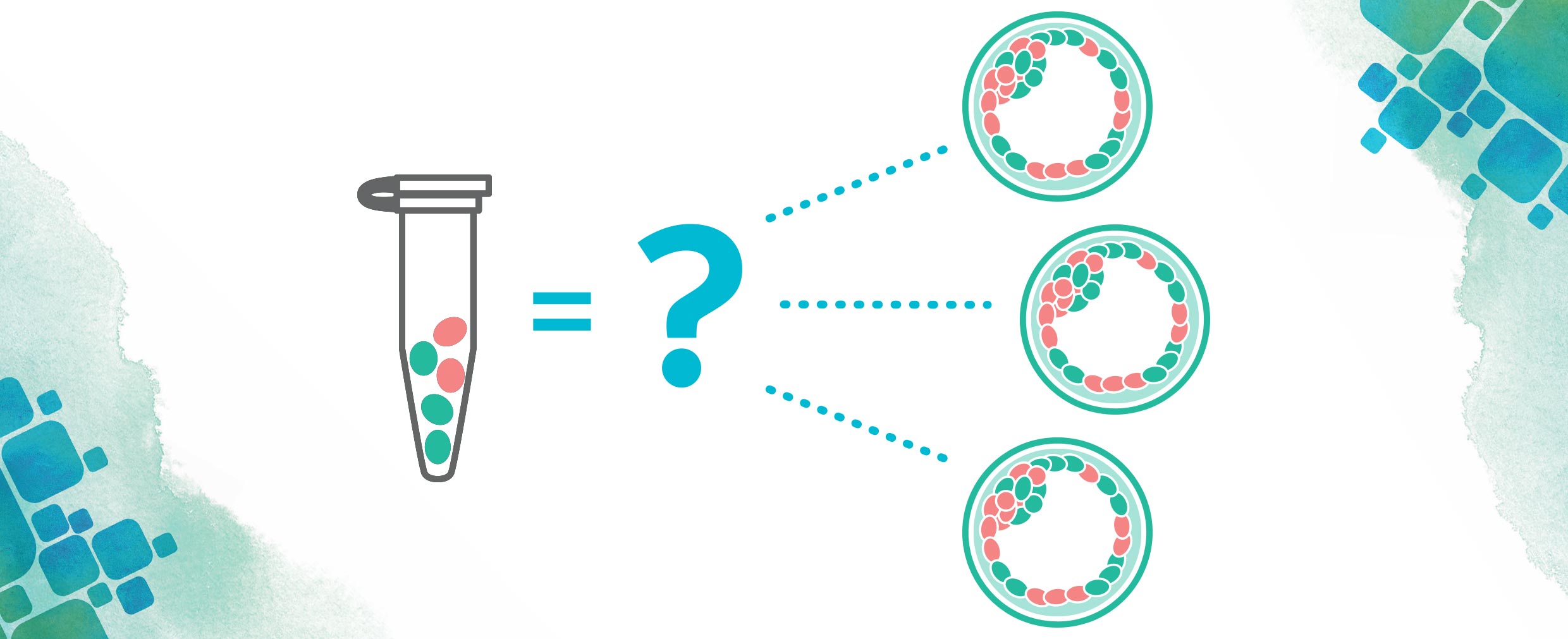
So, what about after fertilization? Is anything else done? Yes, other steps can take place after the embryos are fertilized. Another common reason couples pursue IVF is to screen embryos for genetic conditions the reproductive couple are known to be at risk for. When it comes to embryo selection, some couples may seek additional information to help guide them. Preimplantation genetic testing (PGT) can be done by testing a few cells from embryos. PGT is generally broken up into three different tests based on what is being screened for: aneuploidies, monogenic/single gene defects, or chromosomal structural rearrangements.
 PGT-A (for aneuploidies) is used to screen embryos to see if they have large chromosome abnormalities. Certain genetic conditions such as Down syndrome or Turner syndrome, are associated with extra or missing chromosomes. On top of that, if an embryo is missing a chromosome, it is more likely to not successfully implant, and if it has an extra chromosome, it is more likely to end in miscarriage.1
PGT-A (for aneuploidies) is used to screen embryos to see if they have large chromosome abnormalities. Certain genetic conditions such as Down syndrome or Turner syndrome, are associated with extra or missing chromosomes. On top of that, if an embryo is missing a chromosome, it is more likely to not successfully implant, and if it has an extra chromosome, it is more likely to end in miscarriage.1
 PGT-M (for monogenic, or “single gene,” disorders) is used when a couple knows they are at risk of having an embryo with a condition that is linked to one specific gene. PGT-M can also sometimes be done for small inherited chromosomal deletions and duplications. PGT-M may tell us which embryos are affected with the disorder, which are carriers, and which are unaffected.
PGT-M (for monogenic, or “single gene,” disorders) is used when a couple knows they are at risk of having an embryo with a condition that is linked to one specific gene. PGT-M can also sometimes be done for small inherited chromosomal deletions and duplications. PGT-M may tell us which embryos are affected with the disorder, which are carriers, and which are unaffected.
PGT-SR (for structural rearrangements) is used to screen embryos for any known chromosome rearrangements known in the reproductive couple, such as inversions, reciprocal translocations, or Robertsonian translocations, that could be passed from parent to child.
PGT and embryo transfer decisions
These tests are meant to guide embryo selection by providing patients and their clinics with additional information to be used before embryo transfer (ET) – the last step of the IVF process. A fresh embryo transfer is when an embryo is transferred back into the uterus during the same IVF cycle. If doing a fresh embryo transfer, these embryos generally cannot be biopsied and tested using PGT methods. When a couple is pursuing PGT, embryos need to be frozen after they are biopsied as the clinic awaits the results. Once the patients and the clinic have decided on which embryos to transfer, frozen embryo transfer (FET) occurs. This is very similar to ET, with the major difference being that the frozen embryos are from a previous IVF cycle and need to be thawed before being placed in the uterus.
IVF can be quite a journey, but breaking down the terminology shouldn’t have to be. For further resources, we recommend:
The American Society for Reproductive Medicine (ASRM) https://www.asrm.org/
European Society of Human Reproduction and Embryology (ESHRE) https://www.eshre.eu/
Society for Assisted Reproductive Technology (SART) https://www.sart.org/
Acronyms:
ART: assisted reproductive technology
DOR: Diminished Ovarian Reserve
ET: Embryo Transfer
FET: Frozen Embryo Transfer
ICSI: Intracytoplasmic Sperm Injection
IUI: Intrauterine Insemination
IVF: In Vitro Fertilization
PGT: Preimplantation Genetic Testing
PGT-A: Preimplantation Genetic Testing for Aneuploidies
PGT-M: Preimplantation Genetic Testing for Monogenic/single-gene
PGT-SR: Preimplantation Genetic Testing for Structural Rearrangements
TTC: Trying To Conceive
OR: Oocyte Retrieval
References
- Viotti M et al. Using outcome data from one thousand mosaic embryo transfers to formulate an embryo ranking system for clinical use. Fertil Steril. 2021 May;115(5):1212-1224.
Taylor Berry
Taylor is a genetic counseling graduate student at Sarah Lawrence College. She received her bachelor’s degree in Biological Sciences at Florida State University in 2017. She has previously worked as a research technologist at Mayo Clinic. While working at CooperSurgical®, she loved helping patients understand the complexities of the PGT process and listening to their IVF journeys. Outside of genetic counseling, she loves going to the beach, reading, and yoga.