For some women going through IVF, the choice of having PGS performed on their embryos is a no-brainer. If they’ve got a few embryos, they might test them all to help pick the one with the best chance at becoming a pregnancy. However, the classic Hamletian dilemma, ‘to PGS or not to PGS’, is not a simple choice for those who receive news that only one of their embryos has made it to the testing stage. After investing time, money, and hope into an IVF cycle, a single surviving embryo can be a huge let-down, which makes some patients question the need to have their embryo tested with PGS. After all, it either takes or it doesn’t, right?
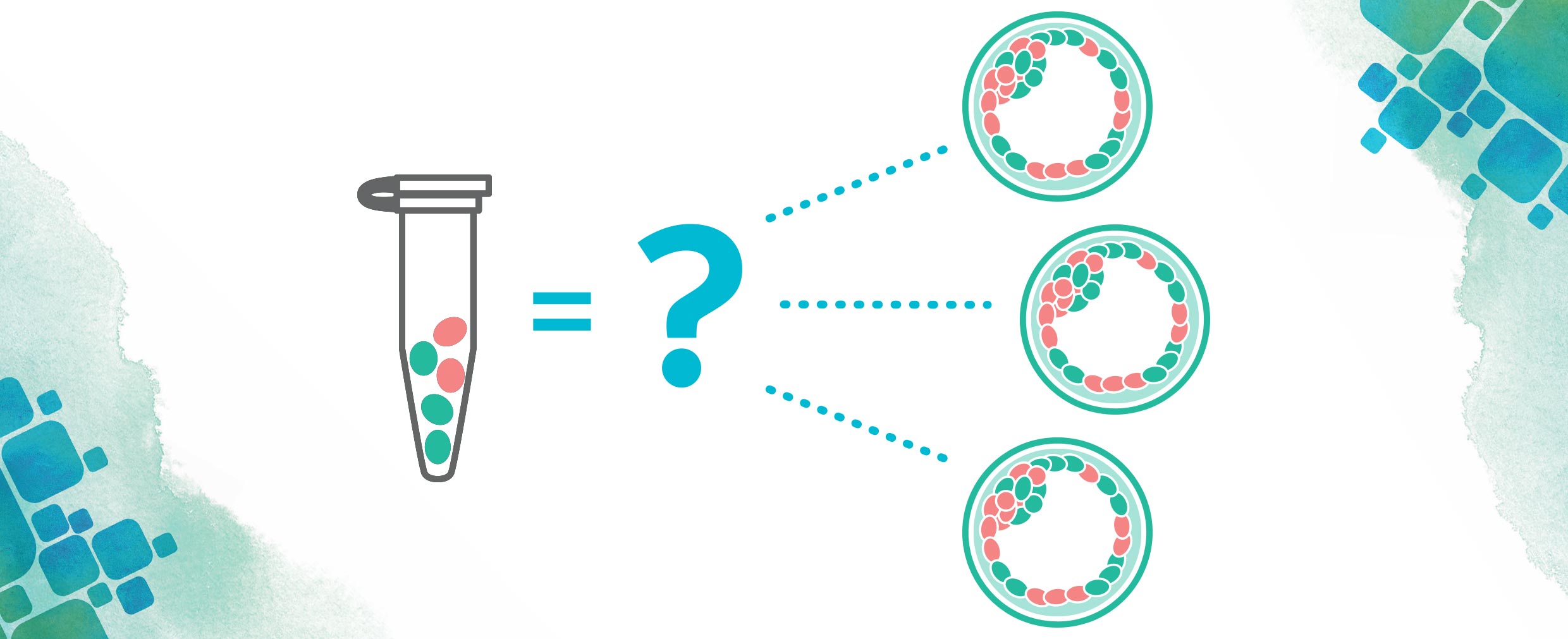
For those new to the terminology, PGS is a genetic test that takes place before embryo transfer, designed to tell you if each embryo is chromosomally healthy. An embryo that is euploid (normal) has 23 pairs of chromosomes and has a better chance at leading to a successful live-birth than an abnormal (aneuploid) embryo. Aneuploid embryos have missing or extra chromosomes and will typically fail to implant, result in a miscarriage, or lead to the birth of a child with a chromosomal disease. Though women with several embryos may use PGS testing to pick the embryo with the best chance at making a baby, for those with only a single embryo available, it’s pretty clear which one you’ll choose. So, is it worth it to test if you only have one embryo? Depending on your specific situation, there are different factors to consider, and we’ve put together a few of them for you here. Every person and every journey is different, and we encourage you to do your research, consult your medical team, and make the decision that is right for YOU.
Your Fertility and Pregnancy History
A journey through IVF is one that is remarkably filled with ups and downs, and every journey is unique. Along with the really high highs (like going through only one cycle and maybe getting pregnant right away), there are some extremely low lows as well. Maybe you’ve lost eggs that never formed embryos, had embryos that never made it to transfer, transferred an embryo that didn’t implant, or possibly (and heartbreakingly) endured the loss of a pregnancy. These losses can leave a lasting impact, and depending on your personal comfort level with the possibility of loss, you may or may not be more open to leaving things up to chance. Because PGS tells you about your embryo’s chromosomal health, an aneuploid result would mean that the embryo either would not implant or would result in a miscarriage. If you’ve already experienced significant loss, the potential emotional cost of another failed transfer or miscarriage may mean that, to you, PGS is worth the extra step. True, you might find out the worst about your embryo, but finding this out before transfer could save you from yet another draining cycle of hope and loss.
Financial Costs
To be completely candid, we all know that IVF is costly. When thinking about whether or not to do PGS, the price tag might be the first thing that comes to mind, and with only one embryo, it may seem like an expensive add-on to an already hefty IVF bill… but the cost factor may not be quite that simple.
Let’s start by envisioning the outcome we’re all crossing our fingers and toes for—a healthy baby. Say you don’t do PGS, and you go straight to transfer. You could end up with a perfectly healthy embryo (and a healthy baby—YAY!), and you’ve saved a little money by opting out of PGS. However, there’s also another potential outcome, should you forgo PGS: you could unknowingly transfer an aneuploid embryo, leading to a transfer that doesn’t take or a pregnancy that ends in loss. You may have saved some money from skipping the PGS testing, but the door is now open for additional costs associated with prenatal care, miscarriage testing, or other medical complications. On the other hand, if you decide to pursue PGS, you will know if your embryo is normal or abnormal before transfer. If your embryo is aneuploid, you will save the cost of transfer, as well as some time if you decide you’d like to cycle again.
Age
If you’re trying to get pregnant after 35, you know (possibly from well-meaning friends and family, ugh) that your biological clock is ticking… loudly. As much as we hate to say it, though, Aunt Ruth actually has a point; not only is it harder to get pregnant the older you are, but the risk for producing aneuploid embryos also increases with maternal age. This remains true regardless of how many embryos are produced–so your single embryo is at just as much risk for aneuploidy as any embryo of yours would be in a cycle where you produced more than one. From the data we’ve seen at CooperGenomics, for women under 35, about half of embryos are euploid, and this number decreases by about ten percentage points every two years. So your age may be a factor in whether you want to do PGS or not, but remember, all women, even those below the 35-year-old mark, have a baseline risk of producing aneuploid embryos.
Other Information You’ll Get from Your Results
Mosaicism
Besides the two possible PGS results we’ve already talked about– euploid and aneuploid– there’s also another: mosaic. A mosaic embryo is comprised of both euploid and aneuploid cells. While mosaicism has existed all along, PGS testing has only been able to recognize mosaicism in embryos within the past three years, so there is still a lot of research ongoing about their potential. What we know now is that about 10-15% of all embryos are mosaic. These embryos aren’t as likely to lead to a successful pregnancy as euploid embryos, but they can sometimes still result in healthy live births. If you decide to do PGS, it is important to know that this is a possible result option. Not all PGS laboratories are capable of detecting mosaicism, so be sure to ask your doctor if this is something your lab offers. CooperGenomics can detect and report mosaicism, and we also have a team of certified genetic counselors who are available at no additional cost to walk you through what this result means and how it can impact your odds of success.
Sex
While the health of your embryo is your number one priority, an added bonus of PGS testing is that it can reveal the sex of your embryo before transfer or pregnancy. This may be important to you for a variety of reasons, and it may be something you’d like to factor into your decision making. If you’d like to know the sex of your embryo, ask your doctor during the discussion of your PGS results. (Note: this may not be available outside of the US.)
Above all, it’s important to remember that genetics, while an incredibly important indicator of embryo health, is only one piece of the IVF puzzle. Many factors contribute to whether an embryo becomes a healthy baby or not, and even transferring a euploid embryo is not a guarantee that you will get (and stay) pregnant, though it does significantly increase your odds. If you choose to undergo PGS, your results can be helpful for making decisions about your personal health, finances, and family building options, and will surely be useful in choosing what next steps to take on your trying-to-conceive journey. Whatever your choice, we wish you the best of luck on the road ahead.