Preimplantation Genetic Testing for Aneuploidy (PGT-A) results
The phone is ringing! After weeks of hormone injections, countless monitoring appointments, one uncomfortable egg retrieval, and days of updates from the embryology lab, you are finally receiving the call you have been waiting for.
You will finally know how many embryos are available for embryo transfer. You answer the telephone and listen intently. Maybe you are taking notes. Immediately, you wish you had a medical dictionary. You may catch a familiar word here or there, but for the most part, these terms are flying right over your head.
What is PGT-A genetic testing?
PGT-A evaluates the chromosome complement of the cells submitted for testing. Chromosomes are the structures that carry all of our genetic material.
Most individuals have 46 chromosomes in each cell of their body. Chromosomes are inherited in pairs; one copy of each pair comes from the egg and one copy of each pair comes from the sperm. The first 22 pairs of chromosomes (the autosomes) are the same in males and females.
The 23rd pair of chromosomes are the sex chromosomes.
Individuals with two X chromosomes are chromosomally female. Individuals with one X and one Y chromosome are chromosomally male.
Got it? Okay! Here is the cheat sheet you need to decipher what you are being told.
Euploid embryos
Pronounced “u-ploid,” euploid means the number of chromosomes observed in the embryo sample was correct at 46. Many times, embryo samples with euploid results will be referred to as “normal embryos.”
Aneuploid embryos
Pronounced “an-u-ploid,” aneuploid means the number of chromosomes observed in the embryo sample was incorrect. There may be extra or missing whole chromosomes, missing or extra pieces of chromosomes (see below), or a combination of these. Often, embryo samples with aneuploid results will be referred to as “abnormal embryos” or have “chromosomal abnormalities.”
Types of aneuploid results:
- Monosomy: mono- means one. In this case, it means one chromosome is present, rather than the expected two (remember, chromosomes are inherited in pairs). As an example, monosomy 7 means that only one copy of chromosome 7 is present in the tested cells instead of the expected two.
- Trisomy: tri- means three. This means three chromosomes are present, rather than the expected two, in the tested cells. A well-known example of a trisomy is Down syndrome. This is caused by the presence of three copies of chromosome 21, rather than two.
- Deletion: a missing piece of a chromosome, rather than an entire missing chromosome.
- Duplication: an extra piece of a chromosome, rather than an entire extra chromosome.
- Segmental aneuploidy: when a chromosome abnormality involves a portion of a chromosome, rather than the entire chromosome. As an example, if the tested cells are missing a portion of the top of chromosome 12, rather than the entire chromosome, this is a segmental aneuploidy.
- Haploid: a single set of chromosomes is present, rather than the expected two, (i.e., there are 23 chromosomes identified rather than 46).
- Triploid: a third set of chromosomes is present, rather than the expected two, (i.e., there are 69 chromosomes identified rather than 46).
- Polyploid: any chromosome result in which an entire extra set of chromosomes is present. Triploid (see above) is an example of a polyploid result, but an embryo sample with four (or more) sets of chromosomes is also considered polyploid.
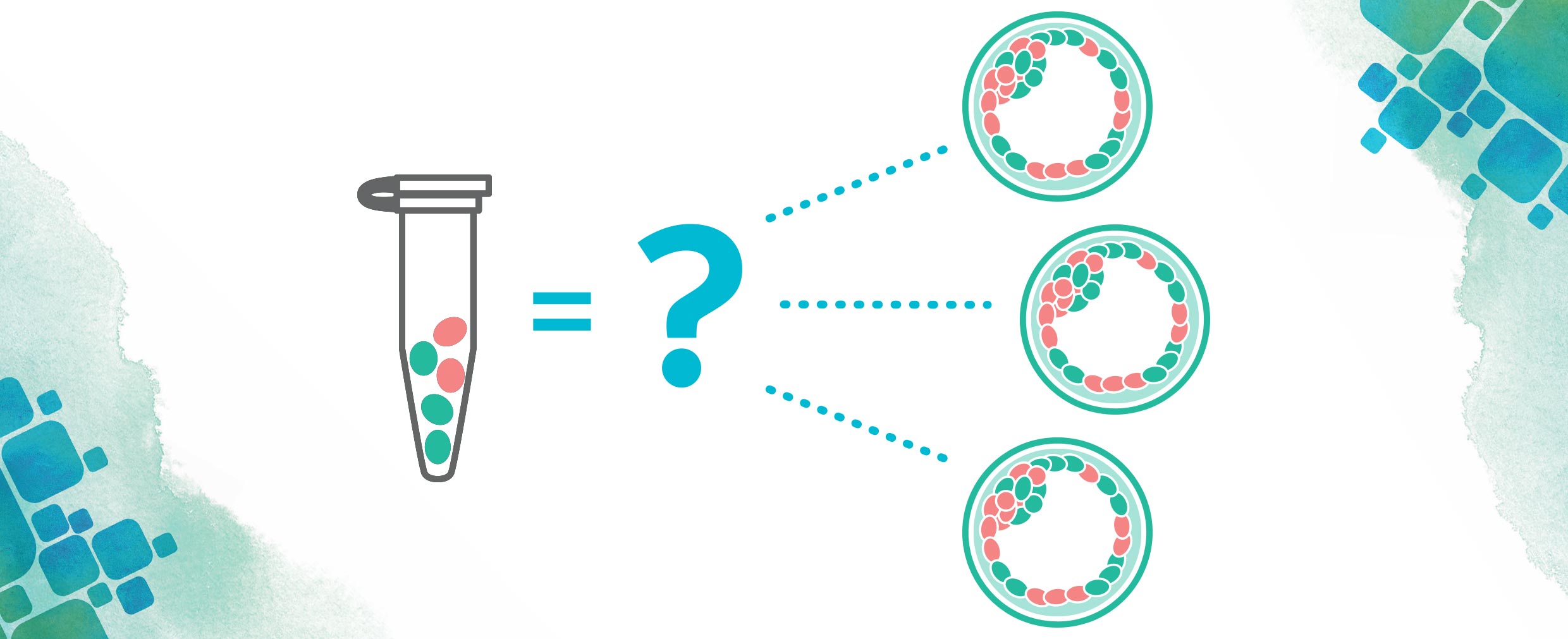
- Mosaic: the presence of two or more populations of cells with different genetic compositions.1 For PGT-A specifically, mosaicism refers to two or more populations of cells with different chromosome complements.
Now that you have the definitions down, here are a couple of other pieces of information that are important to keep in mind when reviewing your PGT-A results.
More information about your PGT-A results
- Don’t be surprised if you have an embryo or two (or more) that has an aneuploid result. Although the risk to conceive an embryo with a chromosome abnormality increases as women age.2 All embryos have a some risk of having an incorrect number of chromosomes, regardless of the age of the mother or egg donor.
- Mosaic results are common and do not appear to be related to the age of the woman or egg donor3, so it is not unusual to have one or more embryos with a mosaic PGT-A result.
- Embryos with euploid PGT-A results have better implantation rates and a lower risk of miscarriage when compared to embryos with aneuploid or mosaic PGT-A results.4,5. However, some embryos with mosaic PGT-A results may result in an ongoing pregnancy and live birth.4,6
Receiving your PGT-A results may be overwhelming. It is common to feel relieved, confused, frustrated, and, in some cases, all of the above. Whatever your results may be, take as much time as you need to digest them.
Do not be afraid to ask your clinicians questions. And do not forget, genetic counseling is available to help you sort through the information. Now, get back to your phone call!
References:
1Nusbaum, RL, McInnes, RR, Willard, HF. Genetics in medicine. 7th ed. Philadelphia: Saunders, 2007.
2McKinlay Gardner RJ and Sutherland GR. Chromosome Abnormalities and Genetic Counseling, 3rd edition. Oxford, Oxford Press, 2004.
3CooperGenomics internal data
4Viotti M, et al., Using outcome data from one thousand mosaic embryo transfers to formulate an embryo ranking system for clinical use. Fertil Steril. 2021 May;115(5):1212-1224. doi: 10.1016/j.fertnstert.2020.11.041. Epub 2021 Mar 6. PMID: 33685629.
5Munne S., et al., Detailed investigation into the cytogenetic constitution and pregnancy outcome of replacing mosaic blastocysts detected with the use of high-resolution next-generation sequencing, Fertility and Sterility, 2018. 108(1): p. 62-71.
6Munne, S, et al., Clinical outcomes after the transfer of blastocysts characterized as mosaic by high resolution next generation sequencing – further insights, European Journal of Medical Genetics, 2020. 63(2): 103741.
About the Author: Sheila Johal
 Sheila Johal is a Manager of Laboratory Genetic Counseling at CooperSurgical; she counsels patients seeking preimplantation genetic testing. She came to CooperSurgical after nine and one-half years at MetroHealth Medical Center in Cleveland, Ohio, where she provided prenatal, general, and cardiovascular genetic counseling. Sheila graduated with a master’s degree in Medical and Molecular Genetics with a focus in Genetic Counseling from Indiana University – Purdue University Indianapolis in 2006.
Sheila Johal is a Manager of Laboratory Genetic Counseling at CooperSurgical; she counsels patients seeking preimplantation genetic testing. She came to CooperSurgical after nine and one-half years at MetroHealth Medical Center in Cleveland, Ohio, where she provided prenatal, general, and cardiovascular genetic counseling. Sheila graduated with a master’s degree in Medical and Molecular Genetics with a focus in Genetic Counseling from Indiana University – Purdue University Indianapolis in 2006.
Prior to attending graduate school, she also received a Bachelor of Science in Biology and a Bachelor of Arts in Psychology from Kent State University. She has a specific interest in disorders of hemoglobin, CFTR-related infertility, and is passionate about educating genetic counseling students. She currently serves as co-chair of the OAGC Web Design Subcommittee. When she is not working, Sheila enjoys being with her husband and children, listening to baseball on the radio, baking, and reading.