I am a statistic. I am one of the 8% of Americans who has a Master’s degree, one of the 24% of American women who serve as the primary income earner in her home and I’m a member of the 12.5% of couples who struggle with infertility.
Every infertility story is unique. No one decides to start a family at exactly the same time nor for exactly the same reason. For my husband and I, our journey started after eleven years of marriage. Until that time, we had been content with our family of three, as my husband has a son from his first marriage. Loving that little boy and helping to raise him was more than enough for me. My husband and I had always agreed that we did not want more children. Then, one ordinary February night, he turned to me and said, “I don’t feel like our family is complete. I want to have a baby.” I’m still not sure if I was more surprised by his declaration, or by my response; a very emphatic, “yes.”
The next day, I did what any good prenatal genetic counselor does. I made an appointment to see my OB/GYN for a preconception visit. I made sure all of my vaccines were current. I started taking a prenatal vitamin with folic acid, and I had my genetic carrier screening. When those results were back, I threw my birth control away.
That first month, nothing happened. Nor the second month. Nor any month after.
I knew something was wrong. I could not explain why I felt that way, I just knew.. After six months, I went to my OB/GYN, who tried to reassure me (she didn’t). I went to a reproductive endocrinologist who told me we had not been trying long enough (for one year).Then she told me that she did not expect to see me again.
Six months, and not a single positive pregnancy test later, my husband and I went back to the reproductive endocrinologist. After a gazillion tests for me, and two (yes, two) for my husband, we had our answer. Severe, unexplained male factor infertility. Our only chance to have a biological child was through in vitro fertilization (IVF).
It’s difficult to describe what receiving a diagnosis of infertility is like. My best attempt is that it feels like an enormous weight is being lifted off of you and at the same time your heart is breaking into a million pieces because of that confirmation and that the journey you are about to embark on may not have a happy ending.
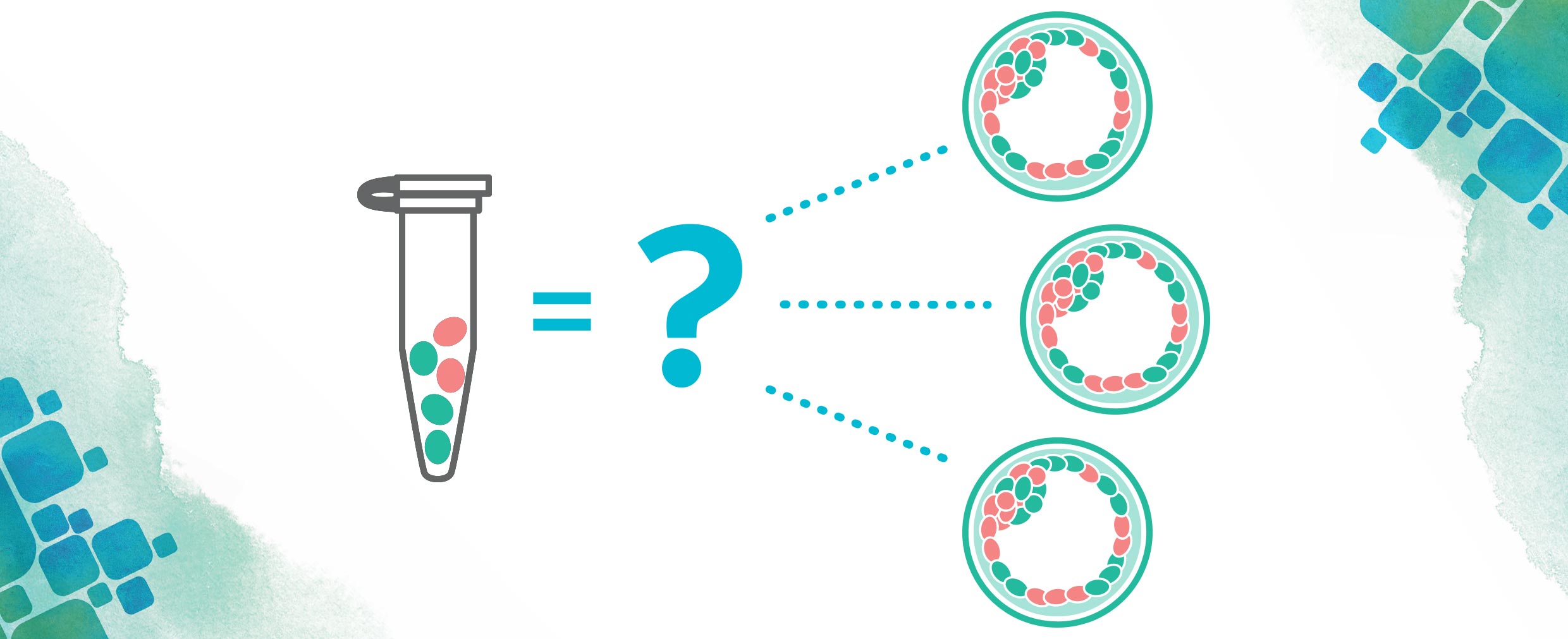
I would love to say that my husband and I were accepting of our diagnosis, and made quick, rational decisions about what to do next. That is not even close to what happened, and I could fill one hundred blogs with details about our reaction to our diagnosis, how it affected our relationship, and how we decided to move forward. The process was long, complex, and filled with emotion. Ultimately, we chose IVF with ICSI (intracytoplasmic sperm injection) and Preimplantation Genetic Testing for Aneuploidies (PGT-A).
We embarked on our first cycle, we were hopeful, excited, and ready to have a baby! Unfortunately, this cycle did not end well. I did not respond well to the medication protocol. I had only ten eggs retrieved, and nine fertilized. The resulting embryos were of very poor quality; so much so that we skipped PGS that cycle because of concern they would not survive the biopsy. We transferred the only two remaining embryos on day 5. Ten days later, I had a positive pregnancy test. Elated understates how I felt. Three days later, it was over. I’d had a chemical pregnancy. It was devastating. I cried for three days, and then I had to rejoin the rest of the world, where no one knew what had just happened.
Three months later, we decided to cycle again. We changed clinics, and my new physician put me on a different ovarian stimulation protocol. I responded infinitely better; with 26 eggs retrieved during that cycle. Sixteen of those eggs fertilized, and on day six we transferred two PGT-A tested normal embryos. Ten days later, I had a positive pregnancy test. I did not let myself get excited because I had been down this road before. But then two days later, my pregnancy hormone had more than doubled. Then, about three weeks later, something resembling a lentil showed up on an ultrasound. Now we have an amazing two-year old son who runs me ragged, and completes our family in a way that we did not even know was needed.
Most of the patients I work with are dealing with infertility. Some of them are at the beginning of their journey, others are seasoned warriors. I do not disclose my history to every patient I work with; it is not usually necessary. However, on occasion, I work with a woman (or a man, or a couple) who is struggling, and it is clear she needs someone to tell her they understand. So, I share my story because I do understand. I have been there, and this is what I know:
I know you are not defined by this. Infertility is one part of you, but it is not all of you. You are an amazing person, who is important to many people. You are worthy of all the love you have in your life.
I know IVF is not for everyone. It is an invasive, time consuming, emotional, and expensive process. The rate of success is not the same for everyone. There are many ways to build a family, and whatever option gives you the family you have been longing for is the right one for you.
I know after receiving a diagnosis of infertility, you will grieve. Like all grief, you will process it as only you know how. You will process it differently than your partner, and that is okay. It is a grief that most others in your life will not understand. If you choose to share your experience, most of those you confide in will be ill equipped to comfort you. Not because they do not want to, but because they do not know how.
And I know that, regardless of how your journey ends, infertility leaves permanent scars. They become less visible over time. You think about them less often. But they are there. I still never know when a pregnancy announcement will take my breath away, when an ultrasound picture will break my heart, or when a baby photo will bring tears to my eyes. Always be kind to yourself, and know that you are not alone. I walk with you always.
About the Author: Sheila Johal
 Sheila Johal is a Manager of Laboratory Genetic Counseling at CooperSurgical; she counsels patients seeking preimplantation genetic testing. She came to CooperSurgical after nine and one-half years at MetroHealth Medical Center in Cleveland, Ohio, where she provided prenatal, general, and cardiovascular genetic counseling. Sheila graduated with a master’s degree in Medical and Molecular Genetics with a focus in Genetic Counseling from Indiana University – Purdue University Indianapolis in 2006.
Sheila Johal is a Manager of Laboratory Genetic Counseling at CooperSurgical; she counsels patients seeking preimplantation genetic testing. She came to CooperSurgical after nine and one-half years at MetroHealth Medical Center in Cleveland, Ohio, where she provided prenatal, general, and cardiovascular genetic counseling. Sheila graduated with a master’s degree in Medical and Molecular Genetics with a focus in Genetic Counseling from Indiana University – Purdue University Indianapolis in 2006.
Prior to attending graduate school, she also received a Bachelor of Science in Biology and a Bachelor of Arts in Psychology from Kent State University. She has a specific interest in disorders of hemoglobin, CFTR-related infertility, and is passionate about educating genetic counseling students. She currently serves as co-chair of the OAGC Web Design Subcommittee. When she is not working, Sheila enjoys being with her husband and children, listening to baseball on the radio, baking, and reading.